From Minority Nurse Magazine, Fall 2008. View the original print article here.
Americans of color are less likely to complete advance directives than their white counterparts. Nurses can play a leading role in educating minority patients about the importance of planning for end-of-life care.
by Barbara Marquand
As a registered nurse and lawyer with training in medical bioethics, Gloria Ramsey, JD, BSN, RN, knew a lot about end-of-life planning. Yet as her mother lay dying in a hospital after suffering a stroke, Ramsey’s knowledge didn’t save her from distress when it came to making final medical decisions for her.
“I will always remember [how my stomach dropped] when the attending physician asked me the question,” she recalls.
Fortunately, Ramsey knew her mother’s wishes and had the support of family members. But what about others, she wondered, who didn’t have a medical background or family to back them up? Today the question fuels her mission to educate minorities about the importance of planning for end-of-life care in advance—before they suffer a serious illness or become incapacitated.
Although most Americans believe patients should have the right to direct their medical treatment at the end of life, less than a quarter of the general population has completed advance directives. And Americans of color are even less likely to have expressed their wishes in writing.
There are two kinds of advance directive documents: a health care power of attorney (also known as a health care proxy), which identifies the person whom patients select to make medical decisions for them if they cannot speak for themselves, and living wills, which spell out patients’ preferences for end-of-life medical treatment, such as the right to refuse life-prolonging care.
“[Advance directives] help avoid the worst thing that can happen—family members left to make agonizing choices because they don’t know what the person wanted,” says Kathy Brandt, MS, vice president of professional leadership, consumer and caregiver services for the National Hospice and Palliative Care Organization (NHPCO). “If you don’t choose for yourself, the choice will be made for you.”
Removing Cultural Barriers
Nurses can make a profound difference by educating patients about the importance of end-of-life care planning. And when it comes to closing the gap of advance directive disparities, minority nurses can play a key role because they bring to the table cultural knowledge and understanding that helps establish trust in communities of color.
“Nurses are on the front lines,” says Paul Malley, president of Aging with Dignity, a nonprofit organization in Tallahassee, Fla., that promotes better care for people facing the end of life. “These are questions people feel comfortable asking a nurse.”
Minorities are less likely to complete advance directives for a variety of reasons, including a lack of access to culturally and linguistically appropriate information. Mistrust of the health care system, misperceptions about advance directives and difficulties in understanding medical terminology can also create barriers.
Given the long history of racism in this country, some older African Americans suspect they will get inferior medical treatment if they complete advance directives. Many of them have not forgotten the infamous 1932-1972 Tuskegee syphilis experiment, in which 399 African American men with syphilis were misled by researchers and were not given the treatment they needed; 128 died of the disease or related complications as a result.
Ramsey, who has conducted research on African Americans’ perspectives on end-of-life planning, says that some black Americans don’t complete advance directives because they believe their families will know what to do when the time comes. Others view end-of-life treatment planning as giving up hope, or giving up on God. African Americans who do complete advance directives tend to request more aggressive life-sustaining treatment than whites.
In the Chinese culture, talking about death is taboo, and Western concepts of end-of-life care, such as hospice, may be unfamiliar to patients who are immigrants from mainland China. Some Chinese elders may have the fatalistic belief that advance end-of-life planning cannot change the future, according to NHPCO, whose Caring Connections outreach program offers informational resources on end-of-life issues developed specifically for Chinese American and Latino populations.
In focus groups with Latinos, NHPCO found that most participants were unfamiliar with the idea of advance health care planning. There were also linguistic misunderstandings about certain terms, such as “caregiver,” which in the Latino community implies a professional role rather than one undertaken at home by family members. Some Latinos have not heard of hospice and may equate it with nursing homes, which have a negative connotation because they go against the traditional cultural belief that it is the family’s responsibility to care for their sick and elderly relatives.
Still other barriers stem from legal red tape. Each state has its own advance directive laws, and some states require advance directive documents to be notarized in the presence of a lawyer. This can be a problem for minorities who live in low-income or rural communities where there is little or no access to notaries and legal services.
“Although the advance directive laws were written with good intentions, they have created hurdles that are insurmountable for many patients,” says Rebecca Sudore, MD, assistant professor of medicine at the University of California, San Francisco.
Simplifying Advance Directives
In a study published in the June 2008 issue of the Journal of the American Geriatrics Society, a team of researchers headed by Sudore recommended that oral advance directives, based on patients’ discussions with doctors, be made legally binding in all states. The study also emphasized the need for health care
professionals and policymakers to facilitate opportunities for discussion about advance care planning in minority communities.
Of the 173 subjects who participated in the study, the majority (73%) were persons of color, and 31% had less than a high school education. The researchers found that subjects who had talked with family, friends or health care professionals about their end-of-life care preferences were more likely to take the next step and complete a written advance directive. Especially in communities where there is distrust of the health care system, says Sudore, the emphasis should be on getting people to think and talk about end-of-life planning rather than looking only at whether they have signed the legal documents.
She also stresses the need for advance directive documents that are easy-to read, easy-to-understand and culturally and linguistically appropriate. In a previous study, Sudore’s research team found that patients in California overwhelmingly preferred a simplified advance directive form to the standard form used in the state. The simplified version, which Sudore created with input from health literacy experts, patients, social workers, nurses and attorneys, uses short sentences, large type and helpful graphics that illustrate the text.
Of the 205 people recruited for the study, 40% had limited literacy and 30% spoke only Spanish. Participants were able to complete greater portions of the simplified form, and almost three-quarters said they preferred it. Six months later, 19% of the group assigned to the simplified form had completed an advance directive for their personal use, compared to only 8% of those who were given the standard form. The simplified form, which is written at a fifth-grade reading level, is now legally valid in California and is available in English, Spanish, Chinese and Vietnamese. (See page 25.)
Other organizations have also been working to make advance directives simpler. In 1998, Aging with Dignity introduced Five Wishes, an easy-to-use advance directive written in plain language. The document includes a health care proxy and lets people state their preferences regarding the kind of medical treatment they want or don’t want, how comfortable they want to be and what information they want their loved ones to know.
“It asks all the right questions and doesn’t make any assumptions about where someone is coming from,” Malley says. Five Wishes is valid in 40 states, and it can be used as a helpful guideline in states where the document does not meet legal requirements.
Two years ago, Aging with Dignity launched the 500,000 Wishes campaign, an outreach program designed to raise awareness of the need for advance care planning in minority communities. Funded by a $200,000 grant from the United Health Foundation, the campaign translated Five Wishes into 20 languages—including Arabic, Hindi, Hmong, Somali and Korean—and offered them for free. So far 250,000 have been distributed to individuals, community organizations, hospitals and hospices nationwide—halfway to the campaign’s goal of reaching a half million minority Americans. “Having this type of document available in so many languages is a first,” Malley says.
“It’s written in a positive and loving light,” says Leslie Piet, RN, MA, CCM, a nurse case manager in Bel Air, Md., who distributes Five Wishes to her patients. In some cases, she reads it aloud to patients. A passionate advocate for end-of-life planning, Piet was prompted by the 2005 Terri Schiavo right-to-die case to host a “living will party” for her family and friends. People gathered to discuss end-of-life choices and complete the Five Wishes document.
“[In our society,] we plan for bringing our children into this world. Now we need to get into the mindset of preparing for transition from this world,” she says. “When good end-of-life care is done well, patients and their families tend to be at greater peace.”
Positive Messages
To reach people from a variety of cultures, education about advance directives must be framed in a positive way, Piet emphasizes. “It’s not about the things you don’t want. It’s about what you do want.”
Most health care facilities are required by the federal Patient Self-Determination Act of 1990 to inform patients about their health care decision-making rights and ask if they have completed an advance directive. But too often this communication with patients becomes a checkbox item.
“It needs to be about more than policy and procedure,” says Anna Terrell, MSN, RN, BC, a retired nurse in Kansas City, Missouri. “It takes some time to sit down with patients and discuss end-of-life care.”
Before her retirement, Terrell educated nurses on advance care planning, served on her hospital’s ethics committee and worked with the Center for Practical Bioethics in Kansas City to learn more about African Americans’ experiences with end-of-life care. She developed a script to use with hospital patients during the admission summary process and tailored it to each patient’s needs, always mindful of their cultural and religious backgrounds.
“You have to be culturally knowledgeable about how to introduce the subject,” she says. “Many African Americans believe that if you bring up the subject of end-of-life care, you’re trying to rush the death.”
Misunderstandings can occur when doctors and nurses don’t consider the issue from their patients’ perspectives. Gloria Thomas Anderson, LMSW, a social worker in Kansas City, recalls how one of her elderly family members became upset and had to be restrained after a nurse asked if she had completed an advance directive.
“She interpreted that to mean that the hospital staff was trying to put her in a nursing home,” Anderson says. “She had avoided medical treatment for over 20 years, because she feared doctors and hospitals.”
After her relative calmed down, Anderson explained that the purpose of the document was not to put her away or to take things from her, but to make sure her family knew her wishes if she were not able to speak for herself. The woman agreed to complete an advance directive, giving one of her adult children power of attorney over her health care needs.
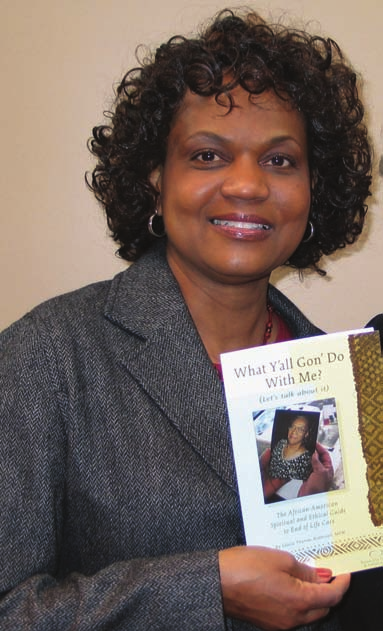
Anderson, who researched end-of-life care for her master’s thesis in 2006, received a grant from the Women’s Council at the University of Missouri-Kansas City to create and produce the booklet What Y’all Gon’ Do With Me? The African American Spiritual and Ethical Guide to End of Life Care. She is now partnering with Kansas City Hospice in a joint effort to distribute the booklet as a free educational resource for African Americans in the Kansas City area. This fall, Anderson will introduce an accompanying outreach training kit that health educators and organizations can use with the booklet to increase awareness of end-of-life issues in the black community.
Forming Coalitions, Building Trust
Collaborating with other health care professionals and organizations can help nurses make an even bigger difference in closing advance directive knowledge gaps in minority communities. Three years ago, Sandy Chen Stokes, MSN, RN, a public health nurse in El Dorado County, Calif., founded the Chinese American Coalition for Compassionate Care to address the lack of linguistically and culturally appropriate end-of-life care information available to California’s Chinese community. Today the coalition includes more than 50 organizations (including NHPCO), provides training for Chinese-speaking volunteers and family caregivers, and offers advance directives, booklets and other educational resources in Chinese and English.
Less than 1% of Chinese Americans have completed advance directives, Stokes says. In focus groups with Chinese American health consumers, the coalition found that many families did not have adequate information for making informed medical decisions at the end of life, and most believed their choices were limited to either aggressive life-sustaining measures or simply “giving up.”
The coalition’s future plans include developing training for health care professionals, expanding its speakers’ bureau and partnering with additional U.S. and international organizations.
“My hope is that [what we are doing in the Chinese American community] can become a model program for other minority groups,” says Stokes.
As part of her research into African Americans’ attitudes about advance care planning, Gloria Ramsey partnered with a large African American church in Harlem, where she provided education on end-of-life issues and advance directives. Ramsey, now an associate professor at the Uniformed Services University of the Health Sciences Graduate School of Nursing in Bethesda, Md., was on the faculty at New York University at the time. She soon realized that even when nurses share the same ethnicity and culture as the community they’re working with, they must still establish trust and credibility before their outreach efforts can succeed.
“Although I am an African American, and the community saw me as African American, I still had to work hard at gaining their trust,” she says. “I had to show that I had no ulterior motives.”
The church was already receiving numerous requests a month to participate in research projects, and it had recently had a bad experience with another researcher. In situations like this, Ramsey advises, “it is imperative to have a local champion, a key person who can [serve as a gatekeeper].”
She partnered with the parish nurse, who acted as a liaison with the pastor and church members. Ramsey also immersed herself in the community by attending services every Sunday and volunteering with the church’s health ministry. She was careful about how she introduced her project. The parish nurse warned her not to use any language about death and dying, for instance.
Ramsey earned the trust of the congregation, although she hit a roadblock early on when she distributed a bulletin insert mentioning organ donation, a question that’s part of the New York advance directive document. The board of trustees, concerned that she was trying to get something from church members through the back door, requested a meeting. Ramsey addressed their concerns and explained her intentions, and the project moved forward. But she says in hindsight she would not have brought up organ donation so soon without first providing education to put the issue in perspective.
Ramsey conducted focus groups and used that input to design a comprehensive, multifaceted health education program for the church. It included information on health risks, healthy living, spirituality and health, grief and bereavement, and advance care planning, using Five Wishes. She also shared her own story of making end-of-life decisions for her mother, which brought the issue home to church members on an emotional level. Suddenly she was perceived as not just an academic but also a loving daughter confronting the challenge of carrying out her mother’s wishes.
Today Ramsey continues to think of her mother as the inspiration for her work. “This was her last gift to me,” she says. “By sharing my story with communities of color, I am able to empower them.”
What Y’all Gon’ Do With Me? The African American Spiritual and Ethical Guide to End of Life Care by Gloria Thomas Anderson, LMSW, can be ordered from her Web site, www.hearttones.com
Barbara Marquand is a freelance writer based in Reno, Nevada.
